In a paper recently published in and featured on the cover of Science, Vodnala and Eil et al. investigated why some patients have dysfunctional tumor-infiltrating lymphocytes (TILs), while others have T cells that behave like stem cells in their capacity to self-renew, proliferate, and destroy large tumors. They found that this difference is driven by the levels of potassium within the tumor microenvironment (TME).
Previous research has shown that T cell differentiation toward an effector state is metabolism-dependent, and that high levels of extracellular potassium cation (K+) – which is released by necrotic tumor cells – within the tumor interstitial fluid in the TME suppress T cell activation and effector function after TCR engagement, independent of PD-1 and CTLA-4. To uncover the mechanism behind this suppression, Vodnala and Eil et al. analyzed the metabolites of T cells conditioned in media with either elevated or normal levels of K+. Elevated extracellular K+ led to reduced nutrient uptake by the T cells despite unaltered extracellular nutrient availability. This functional caloric restriction did not affect T cell survival or proliferative potential.
The metabolite analysis, together with RNAseq and fluorescent confocal microscopy, also indicated that elevated extracellular K+ induced autophagosome formation and maturation, and maintained ongoing autophagy within T cells. Activity of the nutrient-sensing signaling cascades (Akt-mTOR and AMPK) showed that autophagy was induced by a starvation response, triggered by the low nutrient uptake.
In addition to ongoing autophagy, the T cells had enhanced mitochondrial function, which prompted the researchers to take a look at acetyl-coenzyme A (AcCoA). Mitochondrial AcCoA is involved in the citric acid cycle for oxidative phosphorylation, while the nucleocytosolic AcCoA plays a role in histone and non-histone protein acetylation. In the context of elevated extracellular K+, the total cellular AcCoA (a surrogate marker for mitochondrial AcCoA) was elevated, consistent with mitochondria-driven metabolism; however, the nucleocytosolic AcCoA and its precursor citrate were reduced.
Examining the impact of reduced levels of nucleocytosolic AcCoA revealed a crucial role in determining the phenotype and function of the T cell. Decreased nucleocytosolic AcCoA led to decreased histone acetylation and reduced the activation of T cell effector and exhaustion genes, including Ifng, Pdcd1 (PD-1), Cd244 (2B4), Havcr2 (Tim-3), and Klrg1. In contrast to reducing the expression of genes associated with effector functions, inhibition, and suppression of cytolysis, elevated extracellular K+-induced starvation response preserved the expression of genes associated with CD8+ T cell stemness, including the transcription factor Tcf7, the lymphoid homing marker CD62L, and the costimulatory marker CD27. Similar delay in the acquisition of effector functions was observed in CD4+ T cells. To demonstrate a causal link between nucleocytosolic AcCoA and these functional consequences, Vodnala and Eil et al. supplemented the media with AcCoA or its precursor acetate and observed a functional reversal of T cell autophagy, reduction in stem-like properties, and acquisition of effector functions even in the context of elevated K+ levels. In addition, they found that autophagy was required for retaining stemness in the context of elevated K+.
While high potassium levels limit the anticancer activity of T cells in the TME, inducing stemness properties in T cells ex vivo could enhance the effectiveness of T cell-based immunotherapies. In mice with established B16 melanoma, adoptively transferred pmel T cells (which respond to the gp100 antigen) that had been activated in elevated K+ conditions showed improved persistence in the tumor and secondary lymphoid organs; remained in a less differentiated, more multipotent state within the tumor and spleen; and significantly enhanced tumor regression and survival. Secondary transfer of tumor TILs from mice that had received elevated K+-conditioned T cells showed that the TILs had an increased capacity for recall response to antigen, demonstrating that the stem-like state was maintained. Nucleocytosolic AcCoA could be suppressed not only by elevated extracellular K+ levels but also by 2-hydroxycitrate, an inhibitor of a key enzyme involved in the conversion of citrate to AcCoA. Treatment of pmel T cells with 2-hydroxycitrate prior to adoptive transfer affected T cell function in a manner similar to extracellular K+ and led to increased tumor regression and survival in mice with established subcutaneous B16 tumors and pulmonary metastases. Thus, reduction in nucleocytosolic AcCoA, either by a dysregulatory TME or by specific manipulation, preserved T cell stemness.
To determine clinical relevance, the researchers examined neoantigen-specific, tumor-infiltrating T cells from patient tumors (including melanoma and cancers of the colon, lung, and ovary), and surprisingly discovered that exposure to elevated K+ levels led to an increase in the portion of cells expressing CD62L, despite previous chronic exposure to antigen.
Overall, Vodnala and Eil et al. elucidated a mechanism in which elevated extracellular potassium levels within the TME reduced the nutrient uptake by T cells, triggering a starvation response. This caloric restriction resulted in metabolic reprogramming: increased and ongoing autophagy, mitochondria-driven energy production, and depletion of nucleocytosolic AcCoA. Decreased nucleocytosolic AcCoA led to reduced histone acetylation and epigenetic reprogramming, which resulted in reduced acquisition of effector functions and preservation of T cell stemness. The results of this study suggest that ex vivo reprogramming of the metabolic state of T cells could improve the persistence and effectiveness of T cell-based immunotherapies.
by Anna Scherer
Meet the Researcher
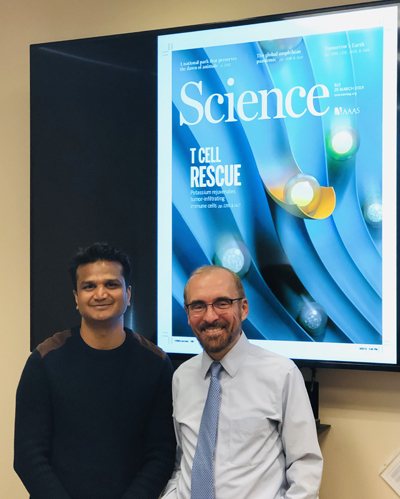
We asked Suman Vodnala, one of the first authors of this study, to tell us a bit more about his research and about himself.
What prompted you to tackle this research question?
From our previous studies we observed that immune cells have differential expression of monovalent transporters and channels to maintain the electrochemical gradients of the cells. We observed that naïve “young”-like T cells have higher expression of these voltage-gated channels and are differentially regulated during their progressive differentiation. This prompted us to study the importance of these channels and the role of monovalent ion’s impact on immune cells.
What was the most surprising finding of this study for you?
The most surprising thing in this study is that a simple ion (K+) can regulate and preserve the essential functions of the cell through epigenetics.
Finally, outside of the lab, what was your recent most exciting “discovery”?
Outside the lab, I custom-design quadcopters and fly them during my leisure time.




