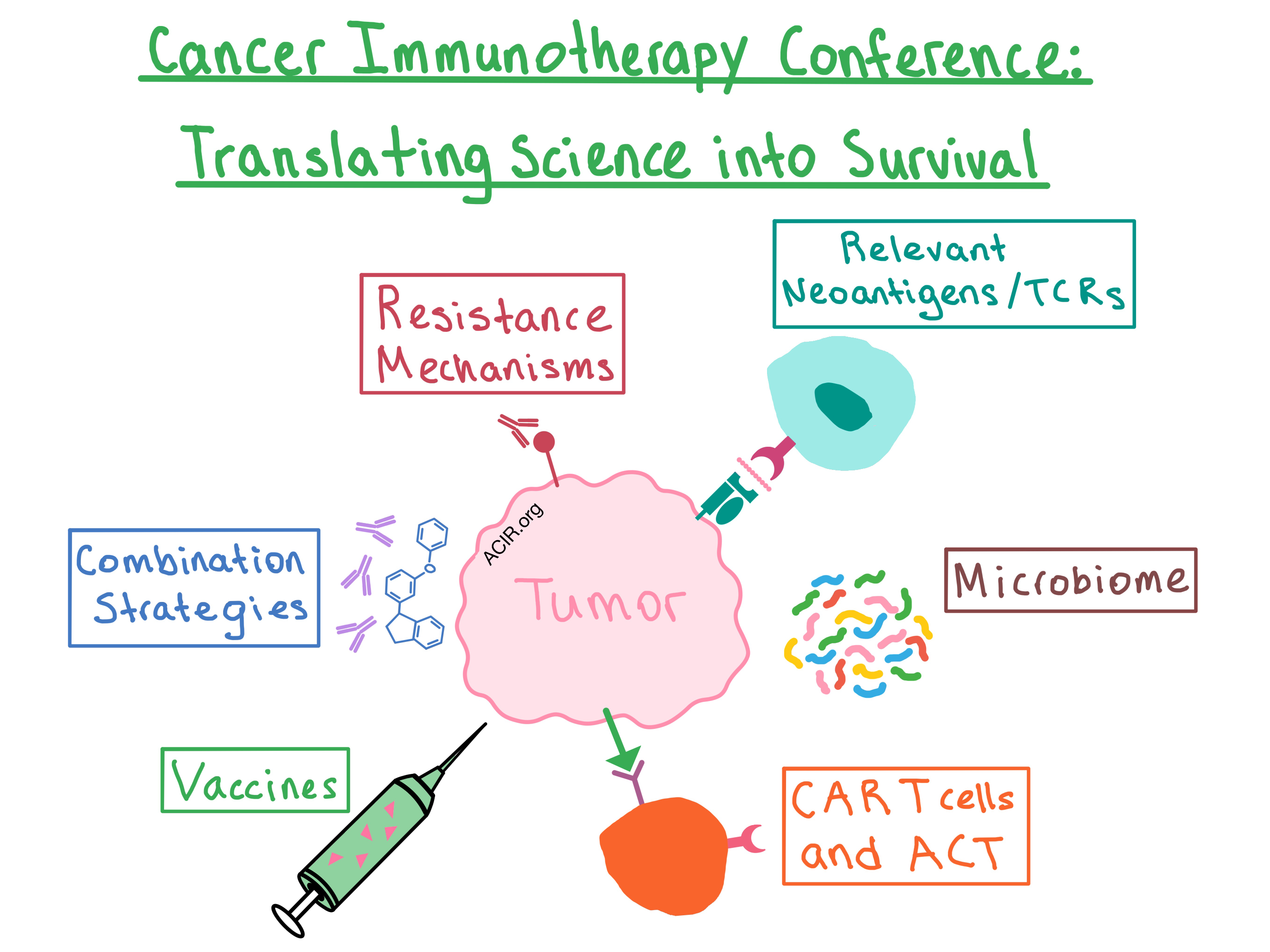
Last week, the ACIR team attended the Fourth CRI-CIMT-EATI-AACR International Cancer Immunotherapy conference in New York. This week’s extensive special feature covers select talks from the conference, which are organized by topics below.
Resistance Mechanisms and Combination Strategies
Identifying Relevant Neoantigens and TCRs
CAR T cells and Adoptive Cell Transfer
Vaccines
Microbiome
Resistance Mechanisms and Combination Strategies
The conference opened with a session on regulating the T cell response to cancer. Nicholas Haining discussed using in vivo genetic screens to discover a novel role for Adar1 (adenosine deaminase that acts on RNA, converting adenosine to inosine), an interferon-inducible enzyme that prevents sensing of double-stranded RNA (dsRNA) and avoids triggering of an immune response. Loss of Adar1 reduced inhibitory cell populations (e.g., MDSCs and M2 macrophages) and increased the population of CD8+ T cells and monocytes within the tumor microenvironment (TME). In addition, Adar1-deficient tumors expressed more IFNβ and IFNγ, and experienced significant growth inhibition. Combination of Adar1 loss and anti-PD-1 synergized to eliminate tumors and prolong survival in mice, and Adar1 deletion resensitized treatment-resistant tumors to immunotherapy, even in the case when tumor cells could not be recognized by CD8+ T cells due to B2m loss. Haining concluded that Adar1 is a checkpoint, and its removal could potentially induce sufficient inflammation to restrict tumor growth while bypassing the need for recognition of tumor by CD8+ T cells.
In another talk, Jake O’Donnell explored the differential effect of using immunotherapy (anti-PD-1 + anti-CD137; other immunotherapies were tested as well) as a neoadjuvant (before surgery) rather than as an adjuvant (post-surgery) therapy. Neoadjuvant use appeared to elicit a more beneficial and durable response in the aggressive 4T1.2 model. O’Donnell showed that this is due to a strong early expansion, subsequent contraction, and establishment of memory response of tumor-specific CD8+ T cells. The memory response originated with previously dysfunctional tumor-specific T cells and did not involve de novo priming. After treatment, tumor-specific T cells from mice treated with neoadjuvant immunotherapy had an increased expression of granzyme B, TNFα, and IFNγ. This translated to reduced tumor growth and increased survival in mice.
Padmanee Sharma presented the William B. Coley Lecture, in which she discussed the response and resistance mechanisms to immune checkpoint blockade (ICB). In order to study the mechanistic pathways triggered by ICB, the researchers conducted pre-surgical or tissue-based Phase Ia and Phase IIa clinical trials to obtain tissue for laboratory examination and development of testable hypotheses in the mouse. Pre- and post-treatment tumor analysis after anti-CTLA-4 treatment demonstrated changes in a number of T cell genes, the most surprising of which was the ICOS pathway. In tumors, antigen-specific functional ICOS+ CD4+ cells were increased, and both ICOS+ CD4+ and CD8+ T cells were increased in the blood of patients. In metastatic melanoma patients increased peripheral ICOS+CD4+ T cells correlated with improved survival. Combining ICOS pathway targeting with anti-CTLA-4 improved survival in mice. In a separate study of patients with metastatic castration resistant prostate cancer, which is poorly infiltrated by T cells, treatment with anti-CTLA-4 converted the TME from “cold” to “hot”; however the expression of inhibitory molecules (PD-L1, VISTA) increased on the newly infiltrating T cells, suggesting the need for targeting multiple pathways in prostate cancer. Dr. Sharma’s main takeaway was that analysis of tumor samples before and after treatment should enable rational guidance for therapeutic decisions.
On the second day of the conference, Ignacio Melero presented the Keynote Address on the importance of IL-8 and CD137 (4-1BB) in immunotherapy. IL-8 (a.k.a. CXCL8) is produced by many solid tumors, where it attracts myeloid cells and potentiates the survival of tumor cells. Clinical trials have shown that for melanoma, NSCLC, or renal cell carcinoma patients treated with anti-PD-1, elevated serum IL-8 at baseline predicted lower survival. Therefore, an IL-8 blocking antibody is being developed for the purpose of combining it with PD-1 blockade. Approaching the response issue from the other direction, Dr. Melero discussed invigorating T cell function using an agonist of the costimulatory receptor CD137, particularly in combination with other immunotherapies, such as ICB or adoptive T cell transfer.
Michelle Krogsgaard explored the mechanisms of primary resistance to PD-1 checkpoint blockade. The researchers hypothesized that when PD-1 is blocked, other inhibitory receptors compensate and alter T cell signaling, therefore limiting response to PD-1 blockade. Using 2D affinity experiments, the researchers showed that the TME impairs TCR affinity to peptide-MHC; PD-1/PD-L1 binding signals via SHP-2, leading to destabilized secondary Lck/Zap-70/CD3 interaction and suppressed TCR-pMHC-CD8 binding. PD-1/PD-L1 blockade recovers the TCR affinity. In non-responders, T cell signaling was altered; therefore, understanding how PD-1 signaling affects TCR binding can help identify additional therapeutic targets that can combine with PD-1 blockade to enhance T cell response.
Identifying Relevant Neoantigens and TCRs
In a session on mutational analysis and predicting response to immunotherapy, Ton Schumacher questioned whether all TILs are actually relevant, and whether focusing on increasing the magnitude and reducing exhaustion of TILs as a whole is the right approach. By using single-cell sequencing to discover TCRs that are reactive against human autologous tumors, and then reconstituting the TCRs in healthy donor T cells to allow for functional testing that is not biased by exhaustion, the researchers showed that most of the identified TCRs were not reactive. They hypothesized that the TCRs were recognizing something other than tumor neoantigens – either immunoedited antigens or non-tumor (viral) antigens at the tumor site. Posing the question as to whether the relevant TILs can be identified without doing TCR sequencing, the researchers found that TILs with high expression of PD-1 predict response to anti-PD-1 therapy (see our feature for more details), suggesting these are the relevant targets.
Stephen Schoenberger discussed an HLA-agnostic method of identifying neoantigens. The researchers performed whole exome sequencing and RNAseq on TILs and PBMCs in combination with bioinformatic analysis to select candidate peptides, and then performed functional T cell assays using autologous PBMCs stimulated with peptides to verify neoantigens. In tumors with low mutational burden, the method produced an average of 35% verifiable neoantigens that induced response in CD4+ and CD8+ T cells. Based on this data, a Phase 1b clinical trial has been initiated to evaluate the efficacy of personalized neoantigen vaccines in solid tumors.
In a session covering the convergence of technology and cancer immunotherapy, Martin Klatt presented a new high-performance HLA ligand identification strategy that enables a more accurate prediction of neoepitope immunogenicity. The method combines the peptide identification algorithm Byonic with the epitope binding predictor netMHCpan. This approach increased identification of unique neoepitope HLA ligands up to 4-fold compared with mass spectrometry.
In another talk, Liang Chen described a way to identify groups of TCRs specific for certain tumor antigens. Current methods focus on counting unique TCR sequences, but do not account for the fact that different TCRs can recognize the same antigen and the same TCR can recognize different antigens. The researchers grouped TCRs by their antigen-binding sites, and found much higher TCR clone convergence in disease than in healthy donor PBMCs.
CAR T cells and Adoptive Cell Transfer
Approaching the impact of the tumor microenvironment on adoptive therapy, Leonid Metelitsa discussed how the properties of NKT cells may be harnessed for cancer immunotherapy. Type-I invariant iNKT cells recognize glycolipids presented on CD1d. In children with stage 4 neuroblastoma, NKT cell infiltration was associated with good outcome. NKTs engineered to express CARs specific for ganglioside GD2 (which is highly expressed in neuroblastoma) more effectively localized to the tumor than CAR.GD2 T cells, and did not induce graft-versus-host disease. Once in the tumor, NKTs selectively and specifically killed tumor cells and the immunosuppressive M2 macrophages in mice. A Phase I clinical trial of autologous NKTs engineered to express GD2-specific CAR and IL-2 for the treatment of children with neuroblastoma has been initiated.
In a session on genetically engineered T cells, Crystal Mackall talked about ways to engineer exhaustion-resistant CAR T cells. Many CAR T cells, with the exception of CD19-CAR T cells, exhibit tonic signaling in the absence of antigen, leading to T cell exhaustion. This is a major limiting factor for the efficacy of CAR T therapies. Another factor in CAR T cell exhaustion is the costimulatory domain, with CD28 predisposing the cells to exhaustion and 4-1BB being partially protective against this effect. Dr. Mackall’s group developed a model to study human T cell exhaustion in a dish, and found that the balance in the expression of activating and inhibitory AP-1 family transcription factors also contributes to CAR T cell exhaustion status. Targeting the expression of such transcription factors may improve the functionality of CAR T cells in the future.
In another talk, Steven Rosenberg discussed targeting unique somatic mutations in cancer using adoptive cell transfer (ACT). ACT has a number of advantages, including the ability to easily grow a high number of antigen-specific T cells and activate them ex vivo, the potential to identify specific cell populations required for cancer regression, and the ability to manipulate the host’s TME prior to transfer to optimize the antitumor effect. Combining whole exome sequencing with tandem minigenes enabled the researchers to identify immunogenic mutations and selectively expand neoantigen-specific TILs and peripheral blood lymphocytes in a manner that did not require peptide:MHC binding prediction or tumor cell line growth (a difficult task for most epithelial cancers). Most identified immunogenic mutations were unique to each patient, while only a few were shared. ACT of the selected TILs enabled durable regressions in patients with various types of metastatic cancers (bile duct, colon, cervix, and breast) that were refractory to other treatments.
In a session focused on targeted therapies, David Porter discussed ways to enhance the function of CAR T cells using immune modifiers and combination therapies. In hematological malignancies (e.g. ALL and CLL), the best correlate of response has been the degree of expansion of CAR T cells in patients. Meanwhile, multiple factors may contribute to poor CAR T cell therapy response, including intrinsic patient T cell defects, T cell exhaustion, poor expansion, poor persistence, and poor targeting to the tumor. Thus, combining CAR T cells with immune modifiers may improve response to therapy. In a clinical trial of CTL019 in combination with the kinase inhibitor ibrutinib, relapsed/refractory CD19+ CLL patients experienced a high rate of complete response (follow up is ongoing). Mechanistically, ibrutinib enhanced the proliferation and survival of CAR T cells and reduced PD-1 expression on CD8+ T cells.
In a session on vaccine platforms and combinations, Cornelis Melief discussed combining ISA101 (a clinical grade, long peptide HPV16 E6 and E7 vaccine) with chemotherapy (carboplatin/paclitaxel) for the treatment of patients with late-stage HPV16+ cervical cancer. In a pilot study of 18 patients, combination of the vaccine with chemotherapy was necessary to overcome the suppressive effects of a hostile TME (via depletion of MDSCs). In a subsequent larger Phase 1/2 study with 70 patients where the timing of the two treatments was optimized (3 vaccinations during 6 chemotherapy cycles), the strength of the vaccine-induced T cell response was positively correlated with overall survival. In a separate Phase 2 study, patients with HPV16+ incurable oropharyngeal cancer were treated with a combination of ISA101 and anti-PD-1; the overall response rate was 36%.
In another talk, Robert Seder described the development of SNP-7/8a, a universal, self-assembling, peptide-TLR-7/8 agonist nanoparticle conjugate vaccine platform. This personalized cancer vaccine allowed for incorporation of any neoantigen into the vaccine, regardless of its solubility (particulate antigens are more efficiently taken up by DCs and elicit a stronger T cell response than soluble antigens, but they are often discarded during the manufacturing process). The polymer formulation demonstrated reduced TLR-7/8 agonist systemic toxicity. In three different murine tumor models, the vaccine induced a neoantigen-specific CD8+ T cell response and enhanced tumor clearance.
Liang Deng discussed how the antitumor effects of an in situ, inactivated modified vaccinia virus Ankara could be enhanced by deleting two viral immunosuppressive genes (C7L, J2R) and expressing exogenous costimulatory molecules (human Flt3L, murine OX40L). Treatment of mice with the altered vaccine eradicated injected tumors, delayed the growth of non-injected tumors, and prolonged survival. Mechanistically, the vaccine increased the induction of IFNβ, activated CD103+ DCs, and increased tumor-specific CD8+ and CD4+ T cell responses.
In a session on microbiome and metabolism, Hassane Zarour discussed how the gut microbiome could be manipulated to improve the efficacy of immunotherapy in melanoma. The researchers analyzed fecal microbiota in 99 stage IV melanoma responders and non-responders to anti-PD-1 therapy and found that certain species were associated with anti-PD-1 response. To determine the effects of diet on the gut microbiota, the researchers analyzed mice that were fed different diets and found that a fiber-rich diet created a microbiome that was more favorable to anti-PD-1 response than a fiber-free diet. A Phase 2 clinical trial has been initiated to determine the effects of administration of a single anti-PD-1 responder-derived fecal microbiota transplant together with PD-1 blockade in resistant melanoma non-responder patients.
Michael Constantinides discussed the contribution of mucosal-associated invariant T (MAIT) cells (which are enriched in the skin) to immune response. Skin-resident MAIT cells depend on cutaneous microbiota-derived IL-23 signaling in order to proliferate and produce IL-1 and IL-17A, cytokines involved in defense against pathogens. As IL-17A confers a pro-tumor effect, targeting MAIT cells via modulation of skin-resident bacteria may have clinical implications in melanoma.
by Anna Scherer




